Advances in genetic sequencing provide baby with life-saving diagnosis is less than fourteen hours
Precision medicine is the future of medical treatments, with top hospitals across the country adopting new clinical practices that integrate this personalized form of medical care into their treatment paradigms. Precision medicine involves treating patients based on their unique genetic and biological traits instead of prescribing a generalized treatment that is given to everyone with a certain disease or condition.
One of the most influential reasons for the increased application of precision medicine has been the increased ability to perform genetic sequencing. Genetic sequencing is essential to understanding the unique genetic factors that will affect how a patient responds to a drug, or to a particular treatment, and can provide valuable information about conditions a patient may have.
Five years ago, a federal initiative “invigorated” research in precision medicine, including neurology programs at institutions nationwide. At that time, Neurology Today covered a case involving a 15-month-old girl. The doctor was David Goldstein, PhD, who went on to lead the Institute for Genomic Medicine at Columbia University Medical Center.
In an important milestone around that time, whole exome sequencing (WES) led to the diagnosis of Brown-Vialetto-Van Laere syndrome (BVVL), a rare disorder of riboflavin transportation associated with the SLC52A2 and SLC52A3 genes.
At the time, Goldstein predicted important and rapid progress from precision approaches in neurology, and other institutions such as the University of California, Los Angeles (UCLA) Health System and David Geffen School of Medicine were creating and running precision medicine diagnostic services, genomics and other specialized testing services, associated bioinformatics, and biobanking.
Precision Medicine in Neurology at Rady Children’s Hospital
Now, a recent case study, published in The New England Journal of Medicine, describes the case of another infant whose life was saved, in this case, using rapid genetic sequencing. The two-month-old infant was brought to Rady Children’s Hospital in San Diego with new neurological symptoms. The infant’s MRI showed worrisome changes, indicating inflammation of the brain, called encephalopathy. The infant was also exhibiting neurological symptoms and seizure activity.
Doctors probed and learned that 10 years prior, the infant’s sister had a similar set of symptoms that required hospitalization and in-depth testing. Despite the extensive evaluation, the infant’s sister passed away at the age of 11 months without any clear diagnosis ever being established. When the infant was initially brought in to Rady Children’s Hospital, it appeared he would experience the same outcome.
The care team identified that a genetic cause of the patient’s encephalopathy was likely. This was because the infant’s parents were first cousins. “Infantile encephalopathy is associated with approximately 1500 genetic diseases, many of which are clinically indistinguishable but have unique, effective treatments,” the infant’s providers wrote in their case study.
‘Ultra-Ultra’ Rapid Whole Genome Sequencing Used
Mallory Owen, MBChB, a pediatric neurologist involved in the patient’s care, and lead author of The New England Journal of Medicine case study, recounted what happened in a recent interview. “We got a call from the [hospital] medical director who said we have a baby in the NICU who I think might really benefit from having this research protocol, ‘ultra-ultra’ rapid whole genome sequencing.”

This method of whole genome sequencing (WGS), nicknamed “ultra-ultra-rapid sequencing” by the researchers that developed it, is an experimental sequencing method that can provide a genetic sequence of the entire human genome in less than 14 hours. In comparison, rapid sequencing takes several days, and ultra-rapid sequencing can provide results in 30 to 50 hours.
Ultimately, the new method of genetic sequencing provided results sixteen-and-a-half hours after the infant’s blood was drawn and indicated that the patient had an extremely rare mutation affecting how two important vitamins, thiamine and biotin, were produced. Simply providing these two inexpensive supplements through a feeding tube was enough to completely resolve the infant’s symptoms and help him quickly resume a healthy life.
Owen’s work points out that many rare genetic diseases have effective treatments but progress to severe morbidity or mortality if untreated immediately. The encephalopathy case is similar to the Brown-Vialetto-Van Laere case such that, in the latter, lack of another vitamin was implicated and then supplemented to improve the patient’s condition. In these cases, it was sequencing led to actions that improved patient care.
Owen indicated that the difference in time of the new method of sequencing used by Rady potentially allowed clinicians to provide treatment one to two days earlier, reducing the potential brain damage caused by encephalopathy and likely leading to a better outcome than even an ultra-rapid sequencing test would have enabled.
“This [baby] is exactly the reason I chose biogenetics,” said Anna-Kaisa Niemi, MD, a Rady neonatologist and metabolic geneticist. “You always try to find the defect and the diagnosis and if you do, you’re able to start treatment fast. But it’s never happened this fast before.”
Rapid Precision Medicine Network Expanding?
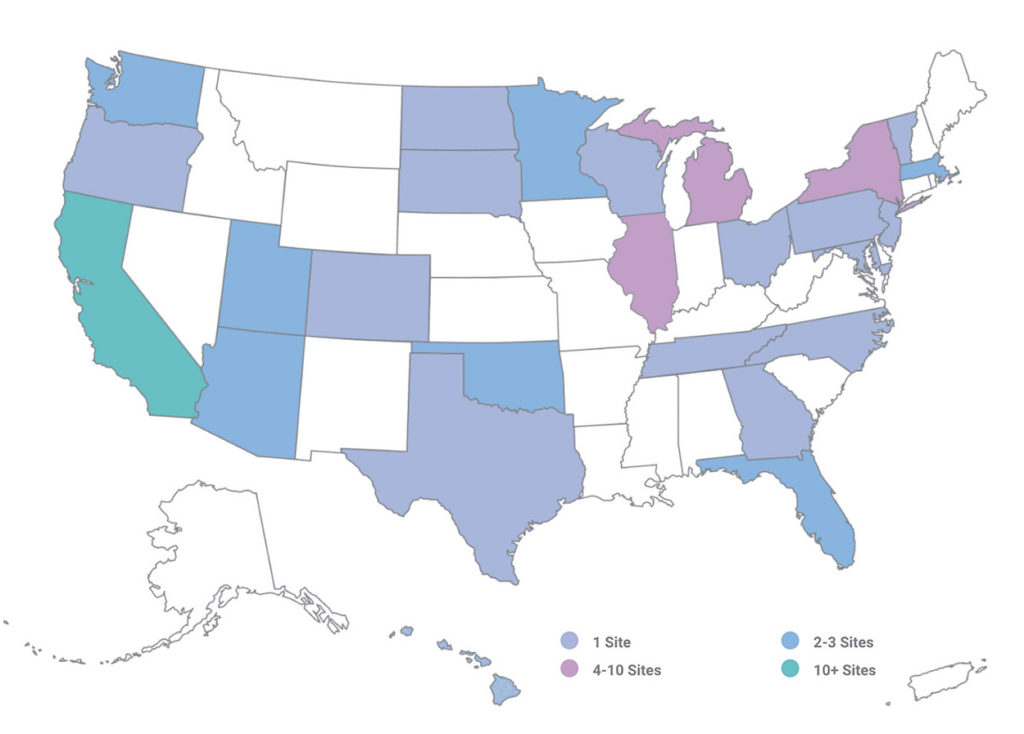
According to its website, the Rady Children’s Institute for Genomic Medicine, which is imbedded within Rady Children’s Hospital-San Diego, has developed an expanding Rapid Precision Medicine Network that provides clinical sequencing and clinical decision support to childrens’ hospitals across the US.
The development of a Rapid Precision Medicine Network, such as that of Rady, is intriguing. It highlights the fact that innovative early adopters are in the best position not only to design new business models but create different brands and perceptions of precision medicine. Other hospital CEOs and their chief medical officers should stay abreast of such developments, and continue to monitor assessments of whole genome sequencing and whole exome sequencing.
Research will continue toward the value and medical necessity of both WES and WGS where results can directly influence diagnostics, medical management, health outcomes, and cost. As a result, payer coverage policies for uses of these high-complexity testing methods are varied and may be changing as more evidence accumulates. By providing rapid genetic results, doctors can more quickly diagnose genetic diseases and can better provide treatments that are tailored specifically to a patient’s unique genotype.
—Caleb Williams
Related Information:
Research at Rady Children’s Hospital
Rapid Genetic Testing May Have Spared This Baby From Death
Rapid Sequencing-Based Diagnosis of Thiamine Metabolism Dysfunction Syndrome
