AI-based technology enables personalized management of chronic and complex conditions at home, potentially reducing unnecessary hospital readmission rates and improving outcomes
Amid the news and noise about telehealth in the US, payers appear to be receptive to coverage depending on services in a given area, including personalized medicine.
In late September just prior to October 13 guidance from the Centers from Medicare and Medicaid Services (CMS) on ending pandemic related waivers and regulatory flexibilities, the US Government Accountability Office (GAO) released some interesting findings with regard to telehealth utilization.
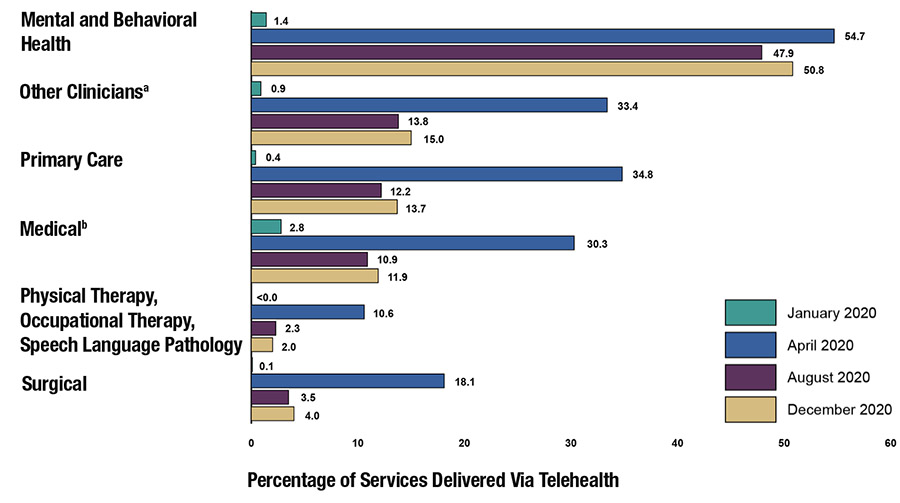
For National Law Review, McDermott Will and Emery penned the GAO’s findings, showing the sharp contrast. Not surprising, as a result of the COVID-19 pandemic, telehealth services appeared to swing from a near resting state between April to December 2019 (five million services) to turbocharged between April and December 2020 (53 million services). Additionally, “5% of providers delivered more than 40% of telehealth services, and 5% of [Medicare] beneficiaries accounted for almost 40% of telehealth utilization.”
Now, the Biden administration must determine where and how to extend regulatory flexibilities beyond the COVID-19 public health emergency. Meanwhile, hospital, health system, and medical device stakeholders continue to make their preferences known, particularly where chronic and complex conditions are concerned.
A Step to Control Costs in Chronic Care Management
In one case, Tennessee-based Community Health Systems (CHS), one of the largest hospital operators in the United States, will provide personalized monitoring and treatments to patients at home. Through a partnership with digital care startup Cadence, announced in February, the service will use artificial intelligence (AI) technology in the form of a digital healthcare monitoring platform. The goals are to avoid unnecessary hospital readmissions and improve health outcomes.
CHS plans to deploy and scale Cadence’s remote patient monitoring (RPM) and virtual care solution across the hospital system’s national footprint, enhancing clinical care for thousands of patients, according to the companies’ joint news release. The program will use AI technology to collect multiple data in patients’ homes, including patients’ vital signs, health histories, and other healthcare data. That data will then be analyzed to create personalized, real-time care plans to better manage chronic health conditions.
“Daily and continuous monitoring at home can improve a patient’s overall health and outcomes and also enable early interventions when necessary,” said Lynn Simon, MD, President of Clinical Operations and Chief Medical Officer of Community Health Systems, as part of the announcement. Community Health Systems is one of the largest publicly traded hospital companies in the US, operating 83 hospitals in 16 states.
CHS’ recent commitment to deploy a new home care technology using AI to provide personalized treatment recommendations will serve as an indicator of current industry trends for healthcare leaders.
“Bringing more healthcare services into the home, using technology to support care delivery, and helping patients manage chronic conditions are imperatives for healthcare systems,” added Tim L. Hingtgen, Chief Executive Officer of Community Health Systems.
At the same time, CHS is also dealing with adjusting operations and consolidating or reducing some services, Fierce Healthcare reported recently. “We will continue to intentionally and aggressively adapt our portfolio services and operations to step over inflationary impacts and other industry headwinds, which we believe will position us for better results in 2023 and beyond,” Hingtgen said during a recent earnings call. “And, we’re supporting our markets with enhanced resources to accelerate growth and revenue, which we know is essential to address fixed and higher variable costs and to restore stronger earnings and margin performance.”
Support for Telehealth After PHE Ends
One of the great lessons from the pandemic is that patients can be monitored based on risk, not on location, University Hospitals Chief Quality and Transformation Officer Peter Pronovost, MD, told McKnight’s Home Care in March.
Researchers at University Hospitals and Case Western Reserve University have said home remote patient monitoring technologies and telehealth should be more widely used after the public health emergency ends.
They advised creating service lines within hospitals, such as emergency medicine to coordinate the use of remote monitoring, reported McKnight’s. They also recommended hospitals have the proper billing mechanism in place to ensure CMS, as well as private insurers, cover the services. Additionally, they said hospitals need to create protocols that would dictate which patients would benefit from in-home monitoring.
Which Patients Benefit Most From Personalized Medicine at Home?
A second example of patients who would benefit from personalized home monitoring is in the care of those facing organ transplantation. In this case, CareDx has tailored specialized testing and patient monitoring to patient groups where organ rejection and hospital readmission are major concerns. Earlier this year the company announced it would expand its HeartCare service to add a new AI prognostic for cardiac allograft vasculopathy (CAV), one of the leading causes of transplant failure.
“We’ve already started to see the benefits of incorporating artificial intelligence to our KidneyCare multimodality offering, so this latest addition to our HeartCare portfolio is in line with our strategy to drive earlier data-driven interventions to reverse long-term mortality trends and sets the stage for the next wave of innovations,” said Reg Seeto, CEO and President of CareDx, in an April announcement.
Future of Telehealth Reimbursement
In “Future of Telehealth Reimbursement,” Modern Healthcare reported that some 43 states and the District of Columbia have laws addressing telemedicine reimbursement for private payers, with 21 mandating payment parity, and that most insurers cover at least some form of virtual service. Additionally, some 30 state Medicaid programs reimburse for remote patient monitoring.
According to CMS, the states with the highest use of telehealth in 2020 included Massachusetts, Vermont, Rhode Island, New Hampshire, and Connecticut. States with the lowest use of telehealth in 2020 included Tennessee, Nebraska, Kansas, North Dakota, and Wyoming. The Federation of State Medical Boards and the Center for Connected Health Policy are among those tracking state-by-state telehealth policies.
Moving forward, what may truly tip the scales in telehealth’s and digital health’s favor is new legislation and medical device user fees, through which the US Food and Drug Administration (FDA) may be able to catch up to the pace of medtech innovation. Scott Whitaker, President and CEO of AdvaMed, a trade organization representing medical technology developers and manufacturers, described recent congressional action as providing for “greater predictability, consistency, and communication between medical technology innovators and FDA.”
In a recent blog, Whitaker said, “Legislative proposals would add value in areas key to promoting better patient outcomes. These proposals include modernizing diagnostic test regulation, streamlining the review of proposed device modifications, and improving the certification of FDA approval to foreign governments. Our industry will continue to urge congressional action on those reforms….”
As healthcare providers know, while enhancing home care offerings for patients could improve overall satisfaction and well-being, as well as reduce unnecessary hospital readmissions, it is care quality and reimbursement from payers that will be key, and payers may still need to be convinced of the value on a regular basis.
More personalized medicine technologies and program strategies will develop. Innovative healthcare leaders should be following these and other moves as they come at a time when hospital-at-home care delivery systems are becoming more common. In this care model, hospitals offer inpatient level care in patients’ homes, using a combination of home visits and remote monitoring to manage each patient’s care.
Ultimately, the financial and care quality impact of remote patient monitoring and telehealth will vary, but RPM has been shown to reduce hospital admissions, length of stay, and emergency department presentations for some patient populations and particular disease conditions. Projects at CHS and other health networks likely will produce evidence that will enhance precision medicine programs.
—Caleb Williams
Related Information:
Updated 10/13/2022: COVID-19 Emergency Declaration Blanket Waivers for Health Care Providers
GAO Releases Report on Telehealth
CHS’ Growth, Margin Improvement Efforts Slowed by Q3’s Rising Costs, Execs Say
U.S. States and Territories Modifying Requirements for Telehealth in Response to COVID-19
Op-ed: New Law Will Help FDA, Medical Technology Industry to Better Serve Patients
Does Remote Patient Monitoring Reduce Acute Care Use? A Systematic Review
